The Power of Incentives: The Story of Electronic Medical Records
In 1999, The Institute of Medicine (IOM) issued a seminal report on the safety of health care in the U.S.: To Err is Human. The IOM noted that up to 98,000 deaths occurred annually as a result of errors in the health care system. They recommended systemic change to improve the safety of the system. One of the recommendations included in the report was to make better use of electronic order entry systems for prescription drugs since handwritten orders were shown to account for a meaningful number of medication errors. Thus began a journey toward more widespread use of electronic medical record systems, with a hope that they would help reduce medical errors and improve the quality and cost effectiveness of care.
In 2004, then-President George W. Bush included the promotion of electronic medical records in his State of the Union address. He set a goal of assuring that most Americans would have electronic health records (EHRs) within 10 years. President Bush’s plan included funding for demonstration projects, the development of common standards and the promotion of EHRs. Despite his ambitious goal and the administrative support for EHRs, by 2008, only 17 percent of health care providers had electronic medical records.
With the enactment of the American Recovery and Reinvestment Act (ARRA) in 2009, a new direction was set for the implementation of electronic health records. ARRA included incentives for health care providers to implement electronic records through a program called HITECH (Health Information Technology for Economic and Clinical Health Act). Significant incentives. CMS estimated that between $14 and $27 billion would be provided over the course of the program. Physicians adopting electronic records in 2011 could receive $44,000 in Medicare incentives over five years. Additional incentives were available for Medicaid EHRs. But, the incentives are only in effect until 2014. For those providers that do not achieve what is known as “meaningful use” of electronic records, there are penalties starting in 2015.
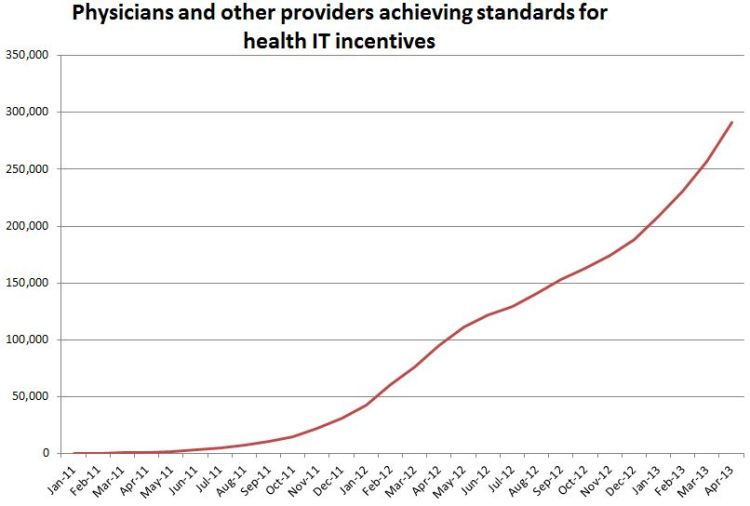
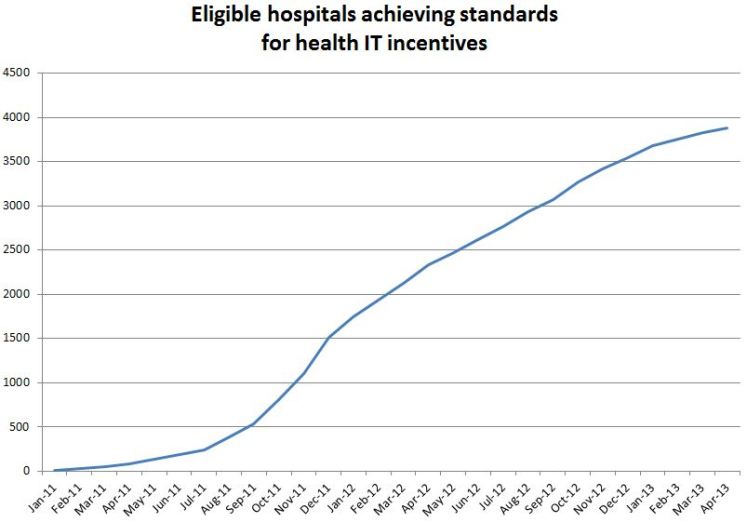
So, what has happened to date as a result of the HITECH program? The U.S. Department of Health and Human Services (HHS) had set a goal of 50 percent of eligible physician offices and 80 percent of eligible hospitals using EHRs by the end of 2013. According to HHS, as of the end of April, 55 percent of eligible office-based providers—or about 291,325 physicians—have received $5.9 billion in incentive payments; and about 80 percent of eligible hospitals and critical access hospitals—or about 3,880 hospitals—have received incentive payments.
Compare those figures to the 17 percent of only five years earlier and look at the graphs in the HHS press release (see further below) and a dramatic picture emerges. If there was ever any doubt about the power of financial incentives to change health care, the HITECH program should set those doubts entirely to rest.
While some physicians still complain about the conversion, there is no question that the HITECH program has been a success in achieving its goals in a way that the prior effort was not. Payers, purchasers and health policy leaders should all take note: establishing a program with clear carrots and sticks (not to mention, the creation of an entire industry geared to respond to this initiative) is an important path forward for dealing with other cost and quality issues in health care.